What Is a Hernia?
A hernia is where an organ or fat protrudes through a weakened spot within the structure of the abdominal wall. The most common type of abdominal hernia is the inguinal hernia, which primarily affects men. The risk increases with age, with the most common sufferers being between 75 and 80 years old.
An abdominal hernia can occur in various regions of the abdominal wall, including the groin, upper abdomen, or near a previous surgical incision. These hernias may present with a visible or palpable bulge, especially when standing, coughing, or lifting heavy objects. While some hernias remain asymptomatic, others may cause discomfort, pressure, or pain.

Table of Contents
- What Is a Hernia?
- Hernia Surgery Specialist: Why Choose Dr. Moein for Hernia Surgery Los Angeles, CA
- What Causes a Hernia?
- What Are Symptoms of a Hernia?
- Hernia Assessment for Tailored Treatment in Los Angeles, CA
- Types of Hernia
- Types of Hernia Surgery Los Angeles, CA
- Benefit of Hernia Surgery
- Hernia Surgery Recovery Time
- Schedule Your Hernia Surgery Consultation in Los Angeles, CA, Today
Hernia Surgery Specialist: Why Choose Dr. Moein for Hernia Surgery Los Angeles, CA

For patients who demonstrate an incidental hernia during bariatric procedures, seeking treatment is often a priority. Dr. Babak Moeinolmolki has the skill and experience necessary to perform hernia surgery at the same time as correct the issue, which is why so many Los Angeles residents, including those from Glendale and Encino, turn to Healthy Life Bariatrics for all of their weight loss needs.
What Causes a Hernia?
Hernias have a variety of possible causes, including:
- Congenital disabilities: Existing at birth, these occur if abdominal wall tissue fails to seal during fetal development properly. This is often the cause of umbilical or inguinal hernias in children.
- Straining: Chronic coughing, constipation with excessive straining to defecate, heavy lifting, or pregnancy/childbirth strain can gradually push tissue through weak spots.
- Prior Surgery: Incisions from past abdominal operations can develop weak scar tissue that gives way later on.
- Obesity: Increased weight places extra pressure on tissues. Fatty tissue more easily pushes through tiny openings.
- Aging: Muscles and connective tissues weaken over time. Men over 45 and women over 60 have higher hernia risks.
What Are Symptoms of a Hernia?
Many people with hernias experience a prominent bulge or lump, but not always. There may also be discomfort or pain. The symptoms may worsen when lifting heavy objects, standing, or straining. Most hernias are diagnosed following a physical test, while others are identified with advanced imaging tools.
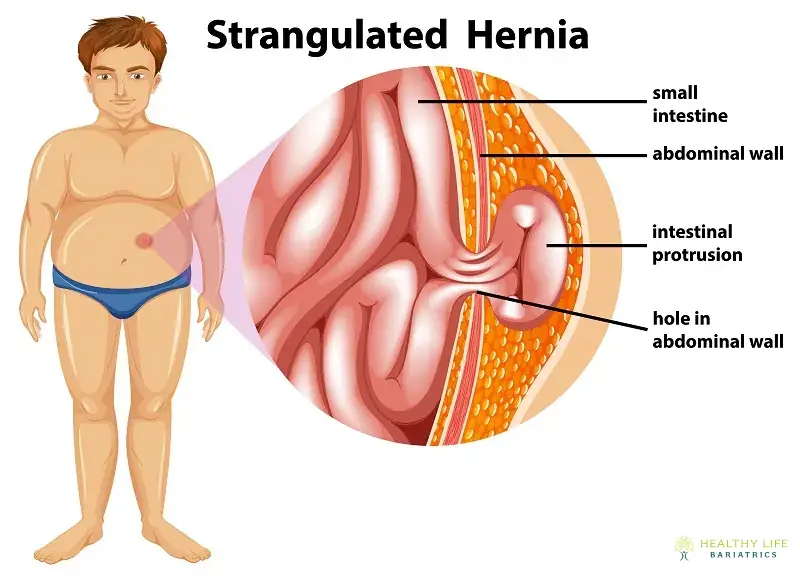
Internal hernias are more complex to diagnose, as there is no visible evidence that something is amiss. Patients with internal hernias often experience abdominal pain. That pain can be located anywhere in the abdomen but is most often focused in the middle part of the abdominal cavity. It might also feel like a burning sensation, tearing, or sharp pain. Left untreated, the discomfort will likely increase as the hernia grows. Patients who are concerned about abdominal pain after a bariatric procedure should contact their surgeon.
Types of Hernia
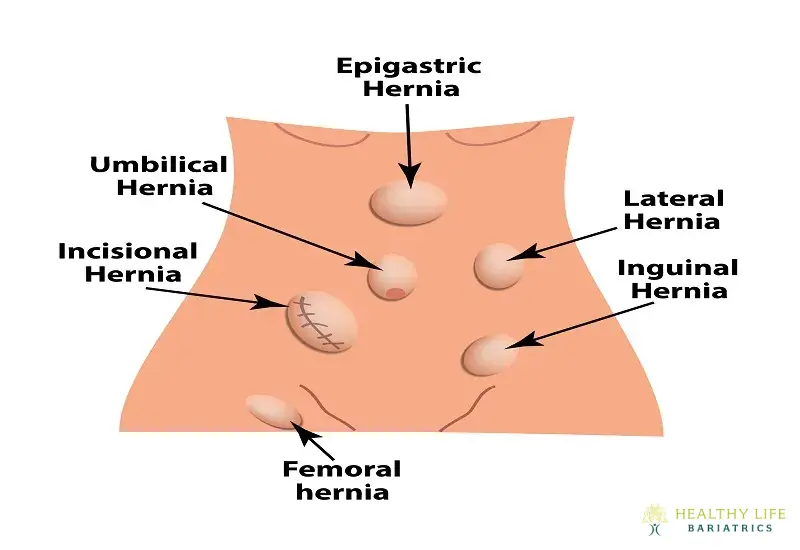
Ventral Hernia
These hernias happen when there is an opening in the abdominal muscles. The three types of ventral hernia include the epigastric hernia, which occurs above the belly button; incisional hernia, which is caused by a weakening of the abdominal muscle resulting from previous abdominal surgery; and umbilical hernia, which occurs near the belly button and is most common in premature newborns.
Ventral hernias can vary in size and severity, and they often present as a visible bulge in the abdominal wall that may become more pronounced with physical activity or straining. While small hernias may remain asymptomatic, larger or symptomatic ones can lead to discomfort, pain, or complications such as incarceration or strangulation of bowel loops.
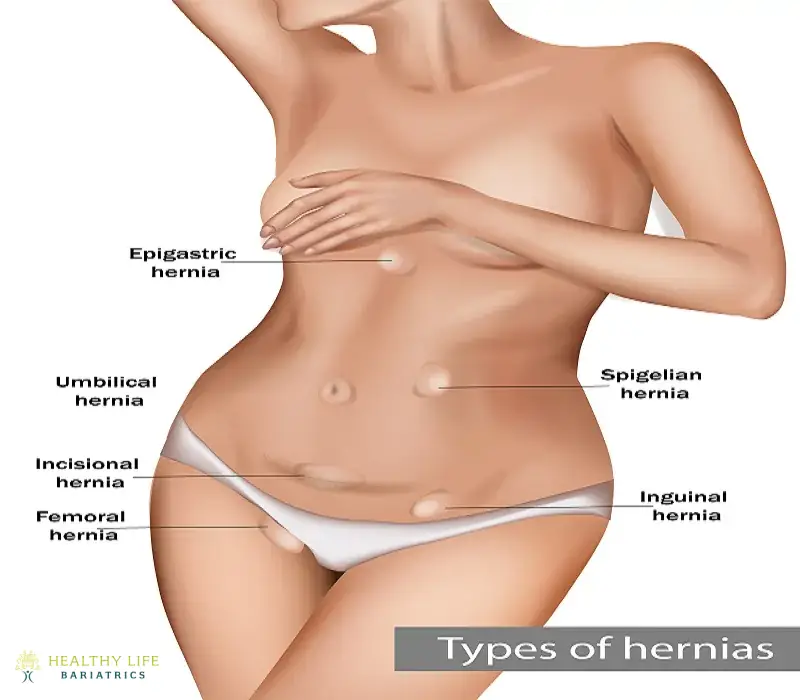
Femoral Hernia
This hernia occurs in the upper thigh or outer groin area and the more profound passages known as the femoral canals. These types of hernias are less common than inguinal hernias and tend to be more common in men. There is a substantial risk of complications if you don't repair the femoral hernia.
Inguinal Hernia
The inner groin area has two passages in the lower abdomen called inguinal canals. An inguinal hernia occurs when the intestine protrudes through either of these two passageways. Experts believe 27% of men and 3% of women will eventually develop this condition.
Hiatal Hernia
A hiatal hernia occurs when the upper portion of the stomach pushes through a small opening in the diaphragm known as the hiatus, which normally allows the esophagus to pass through to the stomach. This type of hernia can cause symptoms such as heartburn, chest discomfort, acid reflux, and difficulty swallowing.
Types of Hernia Surgery Los Angeles, CA
Open Hernia Repair:
The traditional open hernia repair involves an incision directly over the hernia site. Surgeons then push the protruding tissue back into place and reinforce the weakened area with mesh or sutures. Advancements in this technique have led to reduced recovery times and minimized scarring.
Laparoscopic Hernia Repair:
The advent of laparoscopic or minimally invasive surgery has revolutionized hernia repair. This technique entails a few small incisions and a camera to guide the surgeon in repairing the hernia. The benefits of laparoscopic surgery include quicker recovery, less postoperative pain, and a lower risk of infection.
Robotic-Assisted Hernia Repair:
In recent years, robotic-assisted surgery for hernia repair has been gaining popularity. Surgeons control a robotic system to perform the procedure, ensuring greater accuracy in delicate maneuvers. This technique is particularly advantageous in complex hernia cases.
Benefit of Hernia Surgery
Relief from Pain and Discomfort:
Hernia surgery effectively eliminates the persistent pain, pressure, and bulging associated with hernias. By repairing the weakened area of the abdominal wall, the procedure restores normal function and allows patients to return to daily activities—often with reduced reliance on medication and a significantly improved quality of life.
Hernia Surgery Recovery Time
Recovery from hernia surgery in Los Angeles, CA typically depends on the type of procedure performed and the patient’s overall health. Most patients who undergo laparoscopic hernia repair can return to light activities within 3 to 5 days, with full recovery often achieved in 2 to 3 weeks. Those who undergo open surgery may require a slightly longer healing period. Discomfort is generally mild and well-managed with over-the-counter pain medication. It's advised to avoid heavy lifting or strenuous activity for at least 4 to 6 weeks to ensure optimal healing. By following post-operative instructions and attending follow-up visits, patients can expect a smooth recovery and a return to normal function with a low risk of recurrence.
Schedule Your Hernia Surgery Consultation in Los Angeles, CA, Today
Not all hernias cause pain, but a hernia could lead to later complications. Get an official hernia diagnosis and a recommendation for hernia surgery by scheduling a consultation at Healthy Life Bariatrics. Call us throughout Los Angeles, Encino, or Glendale, California, to meet privately with world-class hernia surgeon Dr. Babak Moeinolmolki – at (310)861-4093. Don't wait; take the first step towards a healthier life today!


