
Epigastric Hernias: Causes, Symptoms, and the Importance of Laparoscopic Surgery in Los Angeles, CA
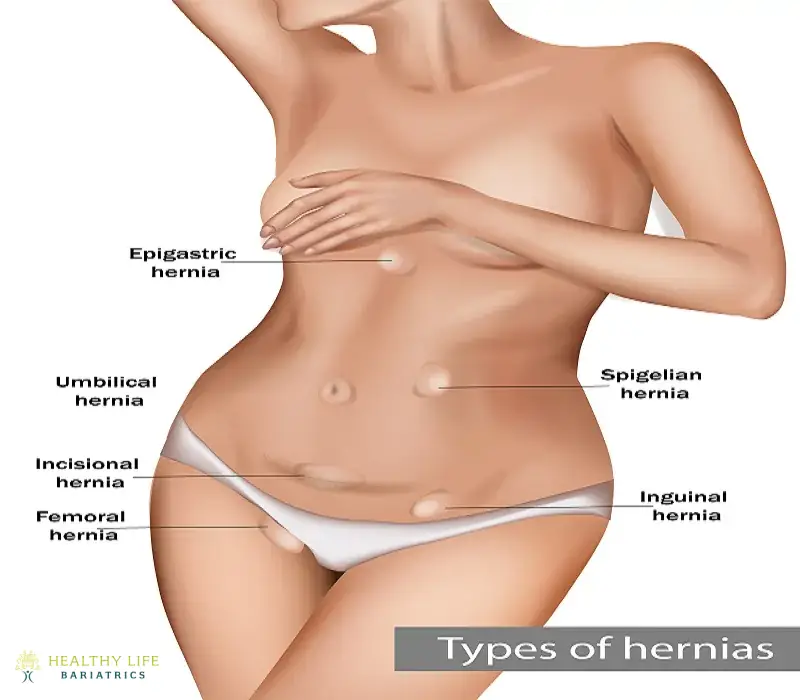
An epigastric hernia occurs when tissue pushes through the inner layers of the abdominal wall, causing a bulge or tear. The hernias can be present at birth (congenital) or acquired. The bulge is usually positioned between the belly button and the chest.
Most epigastric hernias push organs and fatty tissue through the abdominal muscle wall. In minor cases, epigastric hernias don't cause symptoms. Many go undiagnosed and are only discovered during testing for entirely different medical issues. In severe cases, the hernias can cause life-threatening complications.
The recommended treatment for an epigastric hernia is laparoscopic surgery.
General surgeon Dr. Moein offers advanced solutions, including minimally invasive laparoscopic surgery, for patients in Los Angeles, CA, seeking expert care for an epigastric hernia. With extensive experience and a patient-focused approach, Dr. Moein ensures accurate diagnosis and effective treatment to address hernias and prevent complications. If you are experiencing symptoms or have concerns about a hernia, contact Dr. Moein at (310)861-4093 to schedule a consultation and receive personalized care tailored to your needs.
What are the Symptoms of an Epigastric Hernia?
Epigastric hernias seem to come and go at will. This tendency to appear and disappear gives them their nickname: a reducible hernia. The bulge may not be noticeable unless you are having a bowel movement, crying, or engaging in an activity that puts pressure on the abdomen.
A physical exam can usually diagnose an epigastric hernia, while others require advanced imaging technology.
What Causes Epigastric Hernias?
Common culprits enabling epigastric hernia development include:
Prior Abdominal Surgeries
- Any large vertical midline laparotomy incision or periumbilical port sites remaining after minimally invasive operations risk eventual weakening, even decades later.
Chronic Raised Intra-abdominal Pressure
- Obesity, ascites fluid, persistent coughing, or heavy lifting pressures routinely test scar integrity over the years.
Aging Degeneration
- Slow weakening of connective tissue tensile strength through collagenous wear and tear mechanisms.
Trauma
- Significant direct blows harming abdominal wall integrity.
Rare Collagen Disorders
- Inheritable conditions like Marfan or Ehlers-Danlos Syndrome.
Carefully examining patient history illuminates personalized epigastric hernia recurrence risks, guiding treatment decisions to prevent repeat herniations long-term after surgery.
What Symptoms Present with Epigastric Hernias?
Many small epigastric hernias cause occasional vague pain but no apparent external bulging for years. Patients may describe sensations of fullness, cramping, or tightness across the upper abdomen. Eventually, enlarging hernias will elicit:
- Noticeable Bulge – Skin protrusion centers above or near the navel without groin/inguinal involvement. Often enlarges throughout days then reduces somewhat when lying recumbently overnight as gravitational forces temporarily lessen.
- Pain/Discomfort – Aching, heaviness, or perceived muscle strain. Typically exacerbates as hernias expand. Usually reduces with rest and recumbency.
- Pressure – Dull intra-abdominal heaviness, tightness, crammed feeling, or periumbilical pinching.
Significant tenderness, lymphadenopathy, erythema, rapid enlargement, or systemic illness rarely indicate emergent strangulation, as fatty-based epigastric tissues generally preclude vascular compromise like intestinal incarcerations. Still, progressive epigastric hernia expansion eventually risks bowel involvement.
When Should You See a Doctor for an Epigastric Hernia?
An epigastric hernia will not heal on its own. Only surgery can repair the condition. Surgery can be postponed in children until the child reaches an older age. For adults, it's common to be diagnosed with an epigastric hernia that originated earlier in life. The hernia may have been present for years without your awareness. For many, these hernias produce no symptoms until later in life.
Certain conditions and factors can produce epigastric hernia symptoms, such as obesity, strain, and muscle weakness.
You should see a doctor immediately about your epigastric hernia if the tissue protruding through your ab wall gets stuck in an “out” position. Doctors refer to this as an incarcerated hernia. This means the tissue is trapped within the abdominal wall. When this happens, you are at risk for tissue strangulation. That means the intestinal tissue poking through the muscle wall is cut off from its blood supply. Emergency surgery is needed at this stage.

Determining the Best Timing for Epigastric Hernia Repair
The ideal timing for epigastric hernia repair remains to be determined, with mixed data implications. Some clinicians support early intervention upon diagnosis in eligible patients since progressive enlargements increase surrounding tissue attenuation and risks over time. However, other expert consensus guidelines suggest delaying repairs until apparent symptoms develop or hernias approach >2cm large, given the largely benign natural history for those without complicating comorbidities [9]. Customary surgical thresholds include:
- Pain impacts standard activity/quality of life
- Defect diameter reaches 2cm
- Enlargement progression over sequential exams
- Preventing risky future strangulations
How Doctors Diagnose Epigastric Hernias
Visual inspection and palpation during physical exams with patients standing rather than lying down readily confirm small tissue protrusions and reducibility through abdominal wall defects. Imaging tests occasionally help quantify murky pathology:
- Abdominal Ultrasound – Quickly defines fascial disruption zones and hernia dimensions dynamic across positioning.
- CT Scan – Further examines abdominal wall integrity when clinical context warrants.
Overall, most general surgery specialists reliably evaluate epigastric hernias through careful physical examinations alone, assessing for characteristic findings:
- Midline Protrusion – Upper outer quadrant epigastric location remains typical, unlike inguinal involvement. Often enlarges with standing or lean-forward positional maneuvers.
- Positive Cough Impulse – Light finger pressure internalizes tissue bulging at defect sites.
- Smooth Reducibility – Gently maneuvered contents press back in but remain palpable underneath when supine.
The thin body habitus allows for quickly visualizing or photographically documenting how hernias change across standing positions. Heavier individuals require deeper palpations to delineate fascial defects through characteristic cough/pressure rebound signs.
How is Epigastric Hernia Surgery Performed?
Epigastric hernia surgery is performed under general anesthesia. It can be performed inpatiently or outpatiently.
Once the anesthesia has taken effect, small incisions are made on either side of the hernia treatment site. The hernia is repaired laparoscopically, which involves twisting tools that allow Dr. Moeinolmolki to repair your hernia without opening your abdominal cavity. The meticulous surgical techniques are performed while Dr. Moein views the results on a nearby monitor.
Using the laparoscopic camera and associated tools, Dr. Moein isolates the portion of the abdominal lining protruding through the muscle. This “hernia sac” is returned to its proper position before the muscle is stitched closed. Larger holes in the abdominal wall may require a piece of mesh to strengthen the muscle further and prevent future occurrences.
Overview of Epigastric Hernia Repair Approaches
Once bothersome symptoms or progression signs develop, elective surgical reinforcement offers definitive treatment, restoring abdominal wall competency durably. As relatively basic envelope-type protrusions, options include:
Open Epigastric Hernia Repair
Open epigastric hernia repair uses sizeable incisions around defect sites, facilitating maximal exposure for assessing laxity zones and guiding extensive fiber releases before re-approximating midline borders collaboratively with added prosthetic reinforcement. This open approach enables optimal handling of unpredictability but requires more extended hospitalizations and recovery periods [2].
Laparoscopic Epigastric Hernia Repair
Laparoscopic epigastric hernia repair utilizes several small trocar hole incisions in the abdomen for gas insufflation, expanding operative views. Camera-guided minimally invasive instruments then mobilize tissues, facilitating tension-free mesh composite reinforcements across widened defects using sutures/tacks sandwiching layers flatly. Compared to open surgeries, hospital stays shorten dramatically, and patients recover basic activity levels faster despite limitations. However, risks increase slightly for recurrence, chronic discomfort, or mesh complications.
Weighing patient criteria like risks, age, comorbidities, and prior surgeries against hernia characteristics highlights optimal repair techniques for successful outcomes customarily.
Principles of Tension-Free Mesh Hernia Repair
Pioneered in the 1990s, tension-free mesh reinforcement principles revolutionized abdominal wall hernia surgery by patching structural vulnerabilities using macroporous mesh scaffolds with minimized tissue tension during healing phases until surround incorporation strength develops. This facilitated defect bridging regardless of size without pulling on friable skin borders.
Surgeons typically outline fascial gaps by ~5cm zones for mesh graft overlaps on all sides. Composite meshes are then secured by incorporating tissue planes using various fixatives (sutures, tacks, glues) until cellular intermeshing integrates everything cohesively [6]. Patients now convalesce rapidly with minimal lifestyle limitations following such tension-free repairs.
Potential Short and Long-Term Hernia Repair Complications
Despite straightforward envelope type classification and surgery risks remaining relatively low with epigastric hernias overall, possible complications include:
Seroma Fluid Collection – Temporary inflammatory fluid buildup involving recovery areas occasionally needs drainage.
Hematoma Formation – Blood pooling rarely requires evacuation.
Infection – Occurs <1% for small clean cases using antibiotic prophylaxis for hernia surgery. However, higher rates involve larger hernias with more dissection and mesh use, especially with contamination.
Chronic Mesh Discomfort – Acute pain resolves typically within 6 weeks, but neuropathic amplifications cause non-specific aches rarely.
Mesh Dislodgement – Inadequate overlapping with strong fixation until tissue incorporation sets enable migrating, folding, or complete detachments later on.
Hernia Recurrence – Prior infection risks and missed additional defects from limited surgical visualization makes open approaches slightly more durable for epigastric hernia repairs over time based on study reviews.
Progressing appropriate patients towards elective tension-free repairs significantly curtails risks before further deterioration and symptomatic limitations accrue.
What is Recovery Like After an Epigastric Hernia?
Most patients undergoing epigastric hernia surgery can return to their usual routine within six weeks. Your abdomen may feel tender for a week or two. You will want to protect the incision site during recovery, especially when coughing, sneezing, standing, crying, vomiting, and having bowel movements.
Patients feel surprisingly well soon after open or laparoscopic epigastric hernia repairs thanks to anesthetic and therapeutic advancements sparing tissue. Still, gradual loading of healing zones remains imperative for durable long-term construct integrity following principles like:
Early Recovery: Week 1-2
- Using pain medications as needed, weaning as tolerated
- Increasing ambulation with just lifting/straining limits
- Resuming work requiring only light activity in 7-10 days
- Driving once off routine narcotics and able to react normally
Middle Weeks 3-6
- Allowing surgical inflammation and swelling to resolve fully
- Slowly progressing cardiovascular conditioning routines
- Lifting limits remain <25 pounds typically
Late Months 2-3
- Most patients cleared without restrictions by weeks 8-12
- Assessing any lingering discomfort issues
I think following individualized instructions optimizes proper site healing. Most patients see significant improvement after several months, restoring comfortable abdominal wall competency and strength suitably, enabling normal work/life activities without debility fears.
Want to Learn More About Epigastric Hernia Surgery?
A hernia can cause complications over time. Instead of waiting, get an official diagnosis and determine if you are a viable candidate for hernia repair surgery. Call Healthy Life Bariatrics, home of world-class general surgeon Dr. Babak Moeinolmolki, and schedule a consultation at (310) 861-4093.

