How will gastric sleeve help high blood pressure?
Gastric sleeve surgery, a weight-loss procedure that reduces stomach size, can significantly lower high blood pressure by promoting substantial weight loss, which directly impacts obesity-related conditions. When patients experience weight loss post-surgery, excessive body fat—particularly around the abdomen—is reduced, leading to improved blood circulation and lower blood pressure levels.
The surgery also decreases food intake, resulting in a reduction of hunger hormones like ghrelin. Lower levels of these hormones can stabilize metabolism and help patients feel fuller for longer, further supporting weight management. As patients adopt healthier eating habits and lose weight, they often see additional health improvements, including enhanced cardiovascular health and reduced strain on the heart.
Why gastric sleeve might benefit High Blood Pressure
Gastric sleeve surgery can significantly benefit individuals with high blood pressure by promoting substantial weight loss, which helps reduce associated health risks. As patients lose weight after the procedure, they often experience improved blood pressure control—in many cases, leading to a decrease or complete cessation of hypertension medication.
Weight loss resulting from gastric sleeve surgery reduces body fat and alleviates stress on the cardiovascular system, thereby lowering blood pressure levels. This effect not only enhances overall health but also mitigates risks related to heart disease and stroke, which are common among those with high blood pressure.
However, achieving lasting benefits requires commitment to lifestyle changes post-surgery. Adhering to a balanced diet and engaging in regular physical activity are crucial for maintaining weight loss and sustaining improved blood pressure control. Without these measures, patients may miss out on the full spectrum of health advantages.
Other ways to lower high blood pressure
There are several effective non-surgical and non-medication methods to lower high blood pressure. Regular physical activity, such as moderate-intensity exercises like gardening or brisk walking, can enhance heart health and support weight loss, which is crucial for managing hypertension.
Diet also plays a significant role. Adopting dietary patterns like the DASH (Dietary Approaches to Stop Hypertension) or Mediterranean diets, which focus on whole grains, fruits, vegetables, and healthy fats, can effectively reduce blood pressure levels. Reducing sodium intake and limiting alcohol consumption are equally important, as they can help mitigate the strain on the heart.
Stress management techniques, particularly meditation, can help lower blood pressure by promoting relaxation and reducing anxiety. Additionally, biofeedback is another method that may assist individuals in gaining awareness and control over physiological functions, contributing to better blood pressure management.
Regular annual physicals can help monitor risk factors for coronary artery disease, enabling proactive adjustments for a heart-healthy lifestyle. By focusing on exercise, diet, meditation, and weight loss, individuals can significantly lower their hypertension and improve overall cardiovascular health.
The impact of weight loss surgery on patients with high blood pressure
Weight loss surgery significantly impacts patients with high blood pressure by facilitating dramatic weight loss, which can lead to long-term improvements in blood pressure control. Obesity is a major risk factor for hypertension, as excess body fat can cause increased strain on the heart and blood vessels. Following weight loss surgery, many patients experience a reduction in hypertension symptoms and a decreased need for blood pressure medications, with some even achieving remission of their hypertension altogether.
The relationship between obesity and high blood pressure is well-established, making weight loss surgery an effective intervention. Post-surgery, patients usually adopt healthier lifestyle changes, including improved diet and increased physical activity, which further contribute to sustainable weight loss and enhanced health outcomes. These lifestyle modifications are crucial for maintaining the benefits of weight loss surgery, leading to stable blood pressure and a lower risk of cardiovascular complications. In summary, weight loss surgery serves as a powerful tool in managing high blood pressure, addressing the underlying obesity while promoting long-term health improvements.
Gastric Sleeve Effects on Blood Pressure
Gastric sleeve surgery, or sleeve gastrectomy, is a popular bariatric procedure designed to aid significant weight loss by reducing the size of the stomach. Beyond its primary goal of promoting weight loss, this surgery has been shown to have several positive effects on various health conditions, including hypertension, or high blood pressure. As obesity is a major risk factor for elevated blood pressure levels, losing weight through gastric sleeve surgery can lead to substantial improvements in cardiovascular health.
In this context, understanding the relationship between gastric sleeve surgery and its effects on blood pressure is crucial for individuals considering the procedure, as it not only highlights potential benefits but also underscores the importance of lifestyle changes post-surgery to maintain long-term health improvements. The ensuing sections will explore the mechanisms through which gastric sleeve surgery influences blood pressure, the degree of blood pressure reduction observed in patients, and key factors that may affect individual outcomes.
Mid- and Long-Term Effects
Bariatric surgery significantly impacts hypertension, particularly within the first year, when substantial weight loss often leads to marked reductions in blood pressure. Studies indicate that over 50% of patients achieve complete remission of hypertension in the first year post-surgery, with many experiencing reduced medication requirements. However, challenges arise with potential weight regain in the long term, where some patients may experience a resurgence of hypertension despite initial improvements.
Research comparing surgical interventions with conventional medical treatments reveals superior outcomes for hypertension resolution. A study found remission rates of 57% following bariatric surgery compared to only 28% with conventional weight loss methods, underscoring the efficacy of surgical approaches.
However, it's vital to consider both weight-dependent and weight-independent factors influencing outcomes post-surgery, such as changes in metabolic pathways and hormonal regulation. These factors may contribute to improved hypertension control beyond mere weight loss. Therefore, a comprehensive understanding of these dynamics is crucial for optimizing hypertension management following bariatric surgery.

Differences among Surgical Procedures
Sleeve Gastrectomy (LSG) and Gastric Bypass (GB) are two primary bariatric surgical procedures with key differences. LSG is technically easier, involving the removal of a large portion of the stomach to create a sleeve, while GB involves creating a small stomach pouch and rerouting the intestines, which is more complex. Weight loss outcomes are generally similar, with patients losing an average of 60-70% of their excess weight in both procedures. However, GB tends to have higher rates of hypertension remission due to its metabolic effects.
Both procedures come with potential post-operative complications. LSG can lead to gastroesophageal reflux, while GB carries risks of dumping syndrome, malabsorption, and nutrient deficiencies. Gallstones are a common concern in both surgeries due to rapid weight loss.
Ultimately, achieving lasting success post-surgery hinges on significant lifestyle changes, including diet and exercise modifications. Without these changes, patients may struggle to maintain weight loss and improve health outcomes, including hypertension remission.
Metabolic Surgery and HTN
Metabolic surgery, particularly bariatric procedures like sleeve gastrectomy and Roux-en-Y gastric bypass, has a significant relationship with hypertension (HTN). Post-surgery, remarkable physiologic modifications occur, including hormonal changes and improved insulin sensitivity, leading to substantial weight loss. This weight reduction is crucial as it directly impacts blood pressure normalization and the alleviation of comorbidities associated with obesity.
Studies have demonstrated that metabolic surgery can lead to a notable decrease in systolic and diastolic blood pressure, oftentimes allowing patients to discontinue antihypertensive medications. Both sleeve gastrectomy and Roux-en-Y gastric bypass have shown effectiveness in inducing these health benefits, with varying outcomes based on patient selection and specific health profiles.
However, there is a pressing need for standardized definitions of HTN remission and improvement in research studies to comprehensively evaluate these outcomes. Establishing clear criteria will enhance the understanding of metabolic surgery's role in managing HTN and its broader implications for patient health and quality of life. Thus, metabolic surgery stands as a vital tool in addressing hypertension among individuals with obesity, fostering both weight loss and improved cardiovascular health.
Possible Mechanisms Related to HTN Improvement
Hypertension (HTN) improvement following bariatric surgery can be attributed to several interrelated mechanisms, notably involving the renin–angiotensin–aldosterone system (RAAS), glucagon-like peptide-1 (GLP-1), and changes in insulin sensitivity.
Bariatric procedures, such as gastric bypass (GB), alter nutrient absorption and gastrointestinal hormone release, enhancing GLP-1 secretion. GLP-1 promotes insulin secretion and reduces appetite, which can improve insulin sensitivity—a crucial factor as insulin resistance is often linked to elevated blood pressure through RAAS activation.
Post-surgery, reduced caloric intake and weight loss lead to decreased adipose tissue, subsequently lowering circulating angiotensin levels. This decrease diminishes the RAAS's overactivity, resulting in vasodilation and improved blood pressure control. Furthermore, enhanced insulin sensitivity decreases sympathetic nervous system activity, often contributing to HTN.
Cardiac Changes
Obesity leads to significant structural and functional changes in the heart, notably left ventricular hypertrophy (LVH), which is characterized by an increase in left ventricular mass due to the heart's adaptation to increased workload. This hypertrophy often results in impaired diastolic function, where the heart struggles to properly fill with blood. Consequently, individuals with obesity are at a heightened risk of developing heart failure, partly attributable to reduced ejection fraction and impaired filling pressures, as well as atrial fibrillation due to increased left atrial volume and pressure.
Bariatric surgery can partially reverse these detrimental cardiac changes. Post-surgery, weight loss is associated with reductions in left ventricular mass, leading to improved LVH. Furthermore, diastolic function metrics such as the E/A ratio, which evaluates the filling dynamics of the left ventricle, typically show improvement. These adaptations contribute to a lower risk of heart failure and atrial fibrillation, highlighting the importance of weight management in cardiac health.
Vessel Changes
Artery stiffness (AS) is influenced by various factors, notably obesity, which is linked to increased aortic stiffness. Excess body fat leads to alterations in vascular structure and function, contributing to heightened cardiovascular risk. Pulse wave velocity (PWV) serves as a critical measurement tool for assessing AS, where higher PWV indicates greater arterial stiffness and potentially worse cardiovascular outcomes.
Weight loss has been shown to reduce AS, but the mechanisms remain a topic of debate. One theory suggests that weight reduction lowers blood pressure, alleviating strain on arterial walls. Conversely, some argue that improvements in cardiac output may play a more significant role in reducing AS post-weight loss. Additionally, weight loss can lead to reduced inflammatory markers and improved endothelial function, further contributing to enhanced artery health.
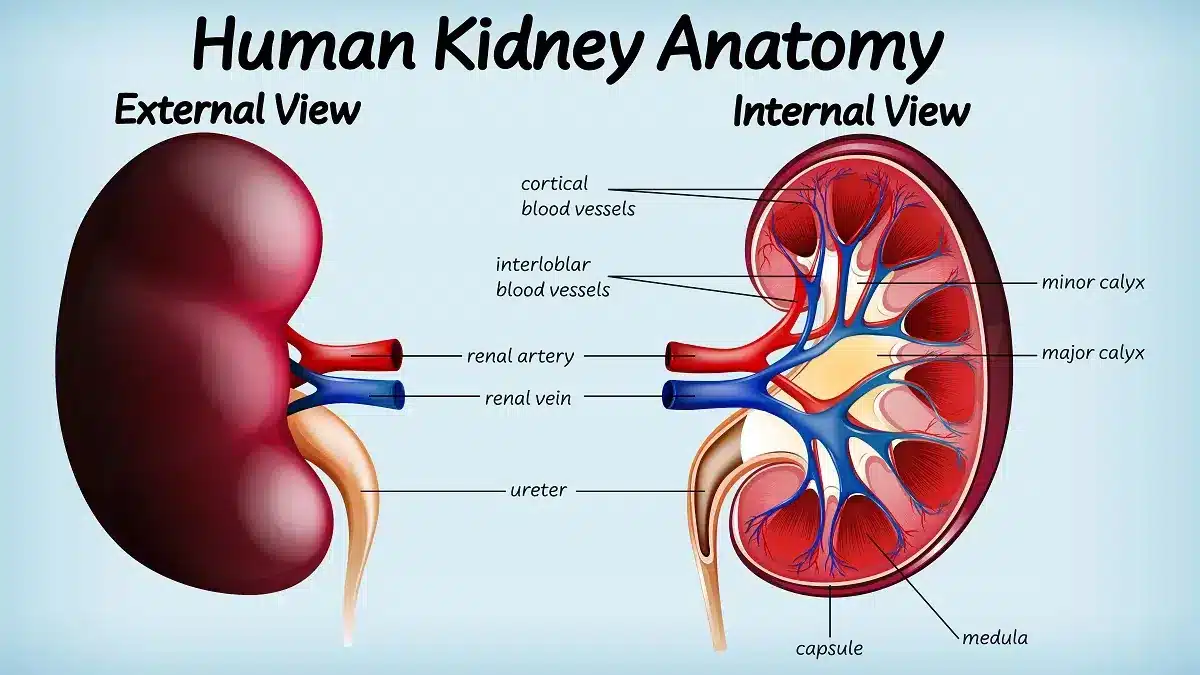
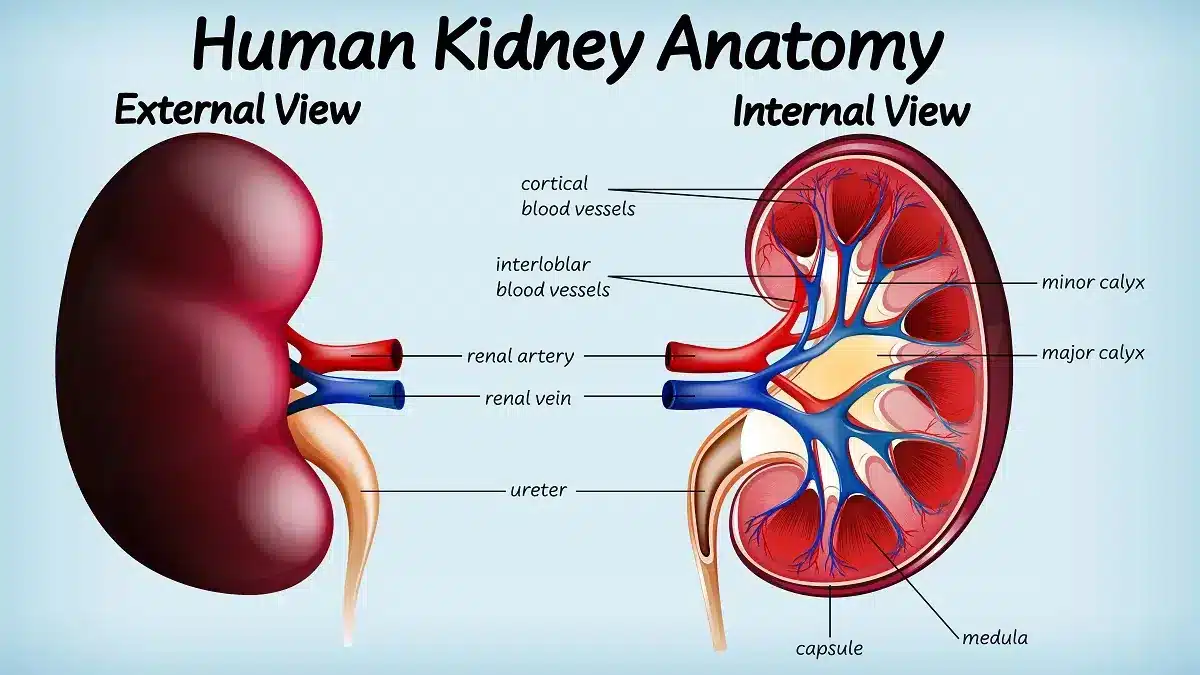
Renal Changes
Obesity induces significant renal changes, primarily characterized by hyperfiltration. Increased adipose tissue leads to elevated levels of circulating inflammatory cytokines, such as TNF-α and IL-6, which exacerbate renal vascular resistance and glomerular hemodynamics, ultimately promoting hyperfiltration. This hyperfiltration state can initiate renal injury through glomerular damage and hypertrophy.
Moreover, renal lipotoxicity, driven by excess free fatty acids, contributes to tubular injury, further amplifying inflammation and fibrosis. Over time, these mechanisms culminate in the progression toward chronic kidney disease (CKD).
Post-bariatric surgery, the accuracy of estimated glomerular filtration rate (eGFR) can be impacted by changes in body surface area (BSA), potentially misrepresenting renal function recovery. Therefore, accurately adjusting for BSA is crucial in post-operative assessments.
Additionally, the presence of albuminuria serves as a critical marker for renal damage, signaling the onset of glomerular permeability changes. Monitoring albumin levels becomes essential in identifying and managing renal injury in obese patients, particularly those undergoing weight loss interventions, to prevent the progression to CKD.
Will Gastric Sleeve Help my High Blood Pressure Summary
Gastric sleeve surgery can significantly improve high blood pressure in obese patients primarily through weight loss and hormonal changes. As patients lose weight after the procedure, the body experiences a reduction in the stress placed on the cardiovascular system, leading to lower blood pressure levels. Additionally, the surgery induces hormonal changes that decrease appetite and improve insulin sensitivity, contributing to further weight loss and metabolic improvements.
Studies have consistently demonstrated substantial reductions in both systolic and diastolic blood pressure post-surgery. However, it's crucial to note that while many patients see positive outcomes, long-term lifestyle changes and ongoing medication may still be necessary to maintain these benefits.
Consulting a qualified surgical and medical team is essential for assessing individual suitability for gastric sleeve surgery. This careful evaluation ensures that patients can achieve optimal results while managing their obesity and related health issues, such as high blood pressure. Overall, gastric sleeve surgery presents a promising option for those looking to improve their health through effective weight loss interventions.