Weight Loss Surgery and Depression: Understanding the Link
Obesity and depression often go hand-in-hand. People struggling with obesity have a 55% increased risk of developing depression compared to the general population.[1] While the exact reasons for this link are still being studied, research suggests that factors like inflammation, altered brain function, and social stigma may play a role.[2]

Fortunately, weight loss surgery, including procedures such as the gastric sleeve, the gastric bypass, and the Lap-Band, offers more than just physical transformation. With proper care, patients often experience emotional healing alongside weight loss. That’s why we provide comprehensive support for both the body and mind at every stage of the journey.
Addressing Depression Before Bariatric Surgery
Individuals considering weight loss surgery should be screened for pre-existing mental health conditions like depression. Studies show that up to 50% of bariatric surgery candidates have a history of depression.[3] Untreated depression before surgery can negatively impact outcomes.
Candidates must receive appropriate treatment to manage depression before undergoing surgery. This may involve therapy and/or antidepressant medication. Getting depression under control beforehand allows patients to be in the best mindset to handle the challenges of surgery and make the lifestyle changes needed for success.
Every patient at Healthy Life Bariatrics undergoes a thorough psychological evaluation before surgery. This is not to disqualify anyone, but to ensure you are mentally and emotionally prepared.
We assess:
Existing depression or anxiety
Coping mechanisms
Lifestyle habits
Support system at home
If needed, we can connect you with licensed therapists or refer you to a bariatric support group for guidance.
How Bariatric Surgery Can Improve Mental Health?
Many patients ask whether weight loss surgery can improve depression. In our experience, the answer is often yes.
Procedures like the gastric sleeve and gastric bypass lead to:
Rapid weight loss
Increased energy
Improved self-confidence
Better mobility and lifestyle
As patients begin to feel healthier and more in control, mood and outlook often improve. At Healthy Life Bariatrics, we closely monitor each patient’s emotional wellbeing throughout the process—from the first consultation through the long-term follow-up phase.
Bariatric Procedures Offered at Healthy Life Bariatrics
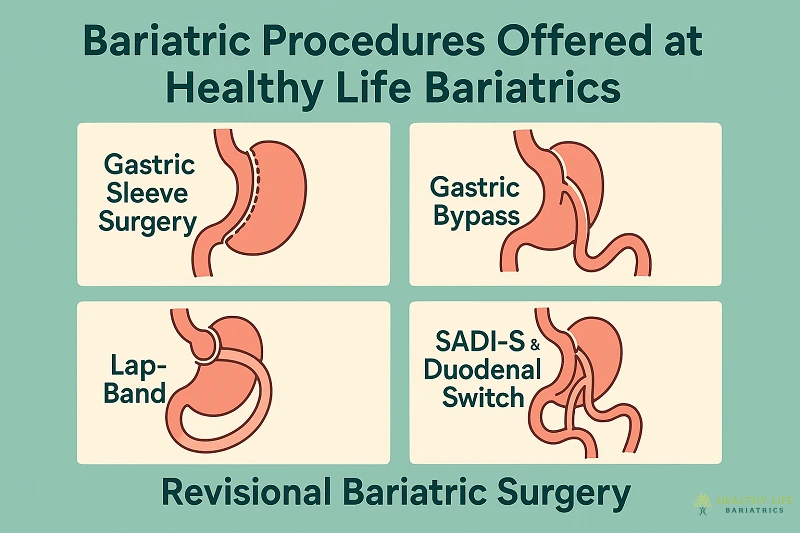
We specialise in a full range of weight loss surgery options, each customised to the patient’s needs and medical history:
Gastric Sleeve Surgery
A restrictive procedure that reduces the size of the stomach to help you feel full faster and consume fewer calories.
Gastric Bypass
Combines restriction and malabsorption by creating a small stomach pouch and rerouting a portion of the intestines, leading to significant weight loss.
Lap-Band Removal or Revision
For patients who have had limited success with the Lap-Band, we offer Lap-Band revision procedures, often converting to a gastric sleeve or bypass for better results.
SADI-S & Duodenal Switch
Advanced procedures for patients with high BMI or complex cases, offering powerful results with careful nutritional support.
Revisional Bariatric Surgery
If you’ve had a previous surgery that did not deliver expected outcomes, we provide expert revision surgery to improve weight loss and reduce complications.
Risk of Depressive Symptoms After Weight Loss Surgery
While weight loss surgery can positively impact self-esteem and quality of life for most patients, some may experience depressive symptoms after surgery. Reported rates vary widely, from 5% to over 50%.[4]
Potential factors include:
- Difficulty coping with rapid change in body image and eating habits
- Nutritional deficiencies like iron, folate, and B12
- Neurochemical changes due to calorie restriction
- Unmet expectations regarding amount of weight lost
- Struggles with maintaining lifestyle changes for weight maintenance
Careful screening and follow-up monitoring for depression should occur for all patients during the first 1-2 years after surgery.[5] Any emerging symptoms should be promptly addressed through support groups, therapy, medication, or nutritional counseling as needed.
Nutritional Deficiencies and Mood
Some emotional symptoms after surgery may stem from nutritional imbalances. That’s why we routinely monitor vitamin and mineral levels.
For example:
Vitamin B12 and iron deficiencies can lead to fatigue and low mood
Vitamin D supports mood regulation and immune health
We customise each patient’s supplement regimen and ensure they receive ongoing lab testing to prevent or correct deficiencies.

Why Choose Healthy Life Bariatrics?
Led by Dr. Babak Moeinolmolki, Healthy Life Bariatrics offers:
✅ Comprehensive bariatric care – from consultation to long-term follow-up
✅ Expertise in all major procedures – including gastric sleeve, bypass, Lap-Band revision, and SADI-S
✅ Psychological support and screenings built into every care plan
✅ Access to support groups, therapy referrals, and nutrition experts
✅ State-of-the-art facilities in Los Angeles, serving Beverly Hills, Century City, and surrounding areas
We don’t just help patients lose weight. We help them reclaim their lives, physically and emotionally.
Schedule a Consultation : Begin Your Journey to Better Health in Los Angeles, CA

It's normal to experience emotional ups and downs before and after weight loss surgery. Having a strong support system is key - this can include friends, family, support groups, and mental health professionals. Patients should be proactive and speak up if they experience symptoms of depression at any point so appropriate treatment can begin right away.
With proper mental health care and self-care, most bariatric patients can successfully manage depression symptoms and experience significant improvements in emotional well-being. Please consider a consultation with Dr. Babak Moein to begin your personal journey.
📞 Call (310) 861-4093 or schedule your private consultation at HealthyLifeBariatrics.com. Together, we’ll design a customised treatment plan that supports both your physical transformation and emotional recovery, for a healthier, more hopeful future.


