After gallbladder removal (cholecystectomy), many patients ask the same practical question: How should I eat in a manner that allows me to regain full vitality promptly and avoid digestive distress? The following in-depth guide provides the essentials of a safe diet after gallbladder removal, including a gradual week-by-week progression, meal planning guidance, and helpful advice that can benefit patients by enhancing digestion, reducing symptoms such as bloating or diarrhea, and enabling them to resume a normal life confidently and safely.

Brief overview: why diet matters after gallbladder removal?
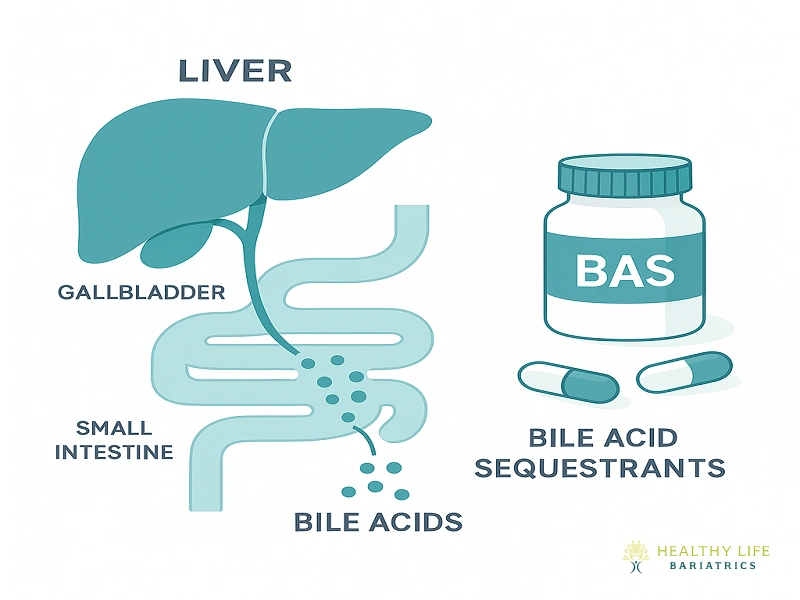
The gallbladder stores and concentrates bile produced by the liver, releasing it into the small intestine to aid in the digestion of fats. After the gallbladder is removed, bile flows directly from the liver to the intestine. Many patients tolerate this change very well, but others may experience temporary changes in fat tolerance and bowel habits. A structured diet after gallbladder removal helps the digestive system adapt, reduces post-operative discomfort, and lowers the likelihood of urgent clinic calls.
Immediate goals after surgery (first 72 hours)
Reduce vomiting and nausea.
Maintain hydration and electrolytes.
Avoid heavy, fatty meals that might invoke biliary-type discomfort or loose stools.
During the early postoperative phase, meals should be small, uncomplicated, and low in fat content. Clear fluids and lightweight, strained broths are tolerated when nausea occurs. When tolerance is enhanced, low-fat, light, easy-to-digest foods may be consumed.
Week-by-week plan: what to eat after gallbladder surgery

Week 1 — Recovery and gentle progression
Aim: control nausea, prevent dehydration, and introduce small, low-fat meals.
Breakfast: plain toast or oatmeal made with water or low-fat milk, accompanied by a small banana.
Snack: applesauce or plain yogurt (low-fat).
Lunch: clear chicken broth, plain white rice, steamed carrots or potatoes.
Dinner: baked or poached white fish (small portion, 2–3 oz), steamed zucchini, and plain mashed potatoes.
Fluids: sip water, electrolyte solutions, and herbal tea. Avoid caffeine and sugary sodas initially.
Tip: Eat 4–6 small meals rather than 2–3 large ones.
Weeks 2–4 — Reintroduce healthy fats slowly
Aim: gradually increase calorie and protein intake while monitoring tolerance.
Introduce small amounts of healthy fats (olive oil, avocado, nut butters) in tiny portions.
Focus on lean proteins, such as chicken breast, turkey, white fish, and eggs (start with half an egg if sensitive).
Vegetables: non-cruciferous steamed or roasted vegetables (broccoli/cauliflower may cause gas — reintroduce slowly).
Grains: whole grains as tolerated — consider oatmeal, whole-grain toast, quinoa.
Dairy: try low-fat yogurts and cheeses; watch for bloating.
Sample day (Week 3): Greek yogurt with honey (small portion), grilled chicken salad with olive oil vinaigrette (1 tsp), baked sweet potato, steamed green beans, and a small serving of brown rice.
1–3 months — Transition to your long-term diet

Aim: adopt a balanced, sustainable diet that supports overall health.
Emphasize Mediterranean-style eating: vegetables, fruits, legumes, whole grains, lean proteins, and moderate healthy fats.
Most patients can reintroduce moderate amounts of fats over time; fried and very greasy foods are best avoided or tested in small quantities.
Pay attention to individual tolerance — some patients may need to limit certain high-fat foods permanently.
Foods to avoid (early and transitional phases)
Fried foods and deep-fried items (French fries, fried chicken).
Very fatty red meats (fatty cuts of beef, lamb).
Full-fat dairy and heavy cream sauces.
Highly processed, greasy, or spicy fast food.
Large portions of nuts, seeds, and high-fat desserts should be consumed immediately after surgery.
Practical meal suggestions and a sample 7-day checklist (short)
Breakfast options: oatmeal with banana, whole-grain toast with a small amount of nut butter, and low-fat Greek yogurt with berries.
Lunch options include chicken and vegetable soup, a turkey sandwich on whole-grain bread with lettuce (no mayonnaise), and a quinoa salad with cucumber and lemon.
Dinner options: baked cod with steamed vegetables, grilled chicken breast with roasted sweet potatoes, and lentil stew (low-fat).
Snacks: rice cakes, bananas, applesauce, plain crackers, low-fat cottage cheese.
Provide patients with a printable 1-page checklist: “Eat small portions, avoid fried foods, chew slowly, keep a food diary for symptoms.”
Tips to manage common post-op symptoms
Diarrhea: Eat binding foods (white rice, bananas, applesauce). Avoid lactose and excess sugar for a few days to allow your body to adjust to the change. If symptoms persist for more than 48–72 hours, contact the clinic.
Bloating/gas: Reduce gas-producing foods initially (such as beans and broccoli), then reintroduce them gradually. Prevent with smaller meals and slow chewing.
Fat intolerance: Reintroduce healthy fats slowly — start with 1 tsp olive oil and monitor.
Supplements, medications, and when to consider enzyme support
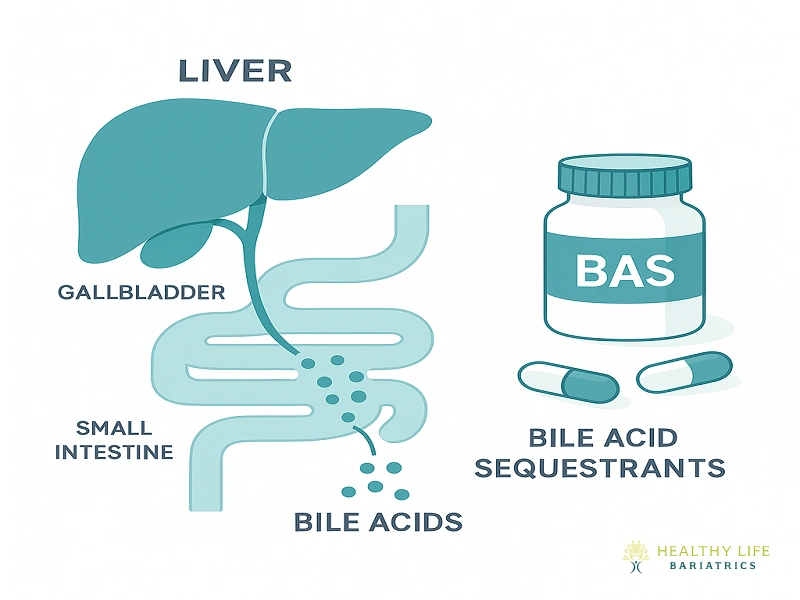
Prophylactic supplementation is generally rarely required after cholecystectomy. When, however, a patient continues to experience signs of fat malabsorption despite adopting appropriate dietary changes and measures, it may then be prudent to consider evaluating a potential underlying condition, such as pancreatic insufficiency or small intestinal bacterial overgrowth. For select situations, temporary supplementation with bile acid sequestrants or adjunctive digestive enzymes may be a therapeutic alternative.
When to call the surgeon or seek urgent care
Advise patients to contact the clinic or go to the emergency department for:
Fever >38°C (100.4°F) or chills.
Persistent vomiting or inability to tolerate any fluids.
Severe abdominal pain not relieved by prescribed medications.
Jaundice (yellowing of skin/eyes), dark urine, or pale stools.
Diet After Gallbladder Removal in Los Angeles — Consult Dr. Babak Moein
Dr. Moein is a board-certified, university-trained surgeon with extensive expertise in both general surgery and bariatric surgery. Dr. Moein is committed to delivering personalized, evidence-based care to each patient, ensuring proper care before and after gallbladder and weigh loss surgical procedures. If you require personal dietary advice, need post-operative surgical follow-ups, or would like to schedule a consultation regarding the types of surgical options available, please don’t hesitate to call our offices at (310) 861-4093. Alternatively, you can use the convenient contact us page.