¿Cómo puede la manga gástrica ayudar con el hígado graso?
La cirugía de manga gástrica, también conocida como gastrectomía en manga, es un procedimiento quirúrgico que puede reducir eficazmente el hígado graso. Este procedimiento implica la eliminación de una gran parte del estómago, lo que da como resultado una bolsa gástrica más pequeña.
El mecanismo de acción de la cirugía de manga gástrica es multifacético. En primer lugar, la cirugía reduce el tamaño del estómago, lo que lleva a una disminución en la producción de hormonas que estimulan el apetito, como la grelina. Esta reducción en las hormonas que inducen el hambre ayuda a las personas a sentirse menos hambrientas y a consumir menos calorías, lo que conduce a la pérdida de peso y a una disminución de la acumulación de grasa en el hígado.
Además, la cirugía de manga gástrica puede tener efectos beneficiosos en el metabolismo de la glucosa. La cirugía altera la comunicación entre el intestino y el cerebro, así como las señales hormonales que regulan la producción de glucosa en el hígado. Esta alteración reduce la producción de glucosa por parte del hígado, lo que mejora el control del azúcar en sangre y disminuye la acumulación de grasa en el hígado.
Varios estudios han investigado los efectos de la cirugía de manga gástrica en la enfermedad del hígado graso no alcohólico (NAFLD, por sus siglas en inglés) y han demostrado consistentemente mejoras en la grasa hepática y la función del hígado. Estudios clave incluyen una investigación realizada por Klein et al. (2006), en la que se informaron reducciones significativas en el contenido de grasa hepática y una mejora en las enzimas hepáticas después de la cirugía de manga gástrica. Otro estudio de Aminian et al. (2018) demostró que la cirugía de manga gástrica mejoró la histología hepática y revirtió la fibrosis hepática en pacientes con NAFLD.
Además, el GLP-1 (péptido similar al glucagón tipo 1), una hormona secretada por los intestinos, desempeña un papel en la mejora de la NAFLD. Los agonistas del receptor de GLP-1, una clase de fármacos que imitan la acción del GLP-1, han mostrado resultados prometedores en la reducción de la grasa hepática y la mejora de la función hepática. Estos medicamentos han sido investigados en varios ensayos clínicos y han demostrado eficacia en la mejora de los parámetros de la NAFLD.

Hígado graso no alcohólico
Hígado graso no alcohólico
La enfermedad del hígado graso no alcohólico (NAFLD, por sus siglas en inglés) es una afección caracterizada por la acumulación excesiva de grasa en el hígado sin la presencia de abuso de alcohol. Se asocia comúnmente con la obesidad, la resistencia a la insulina y el síndrome metabólico. Las causas exactas de la NAFLD son multifactoriales e incluyen factores genéticos, la dieta, un estilo de vida sedentario y ciertas condiciones médicas.
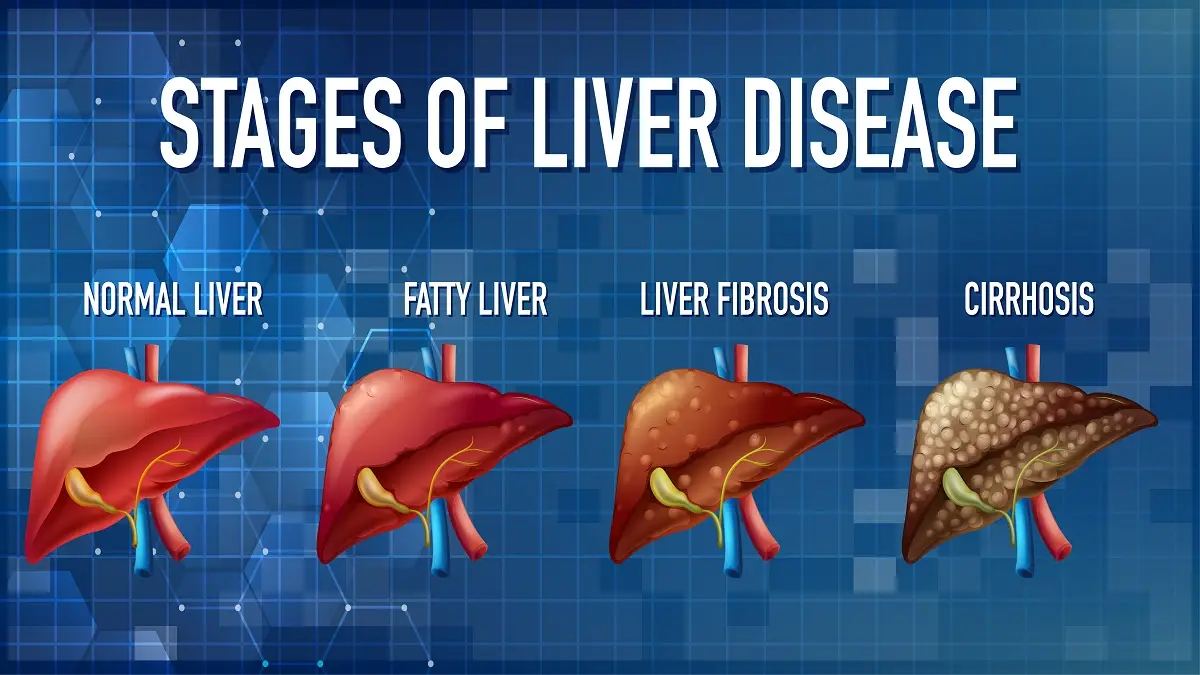
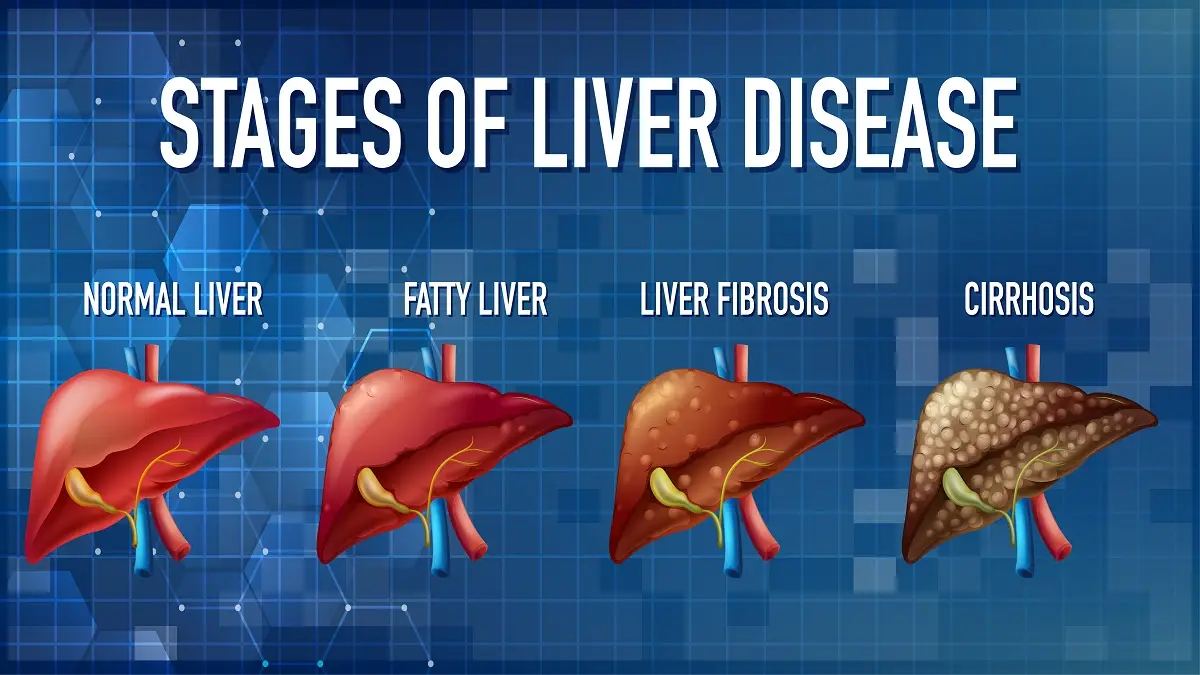
Los síntomas de la NAFLD suelen ser vagos y no específicos, lo que dificulta su diagnóstico en etapas tempranas. Puede haber fatiga, molestias abdominales y leves alteraciones en las enzimas hepáticas. Sin embargo, a medida que la enfermedad progresa, puede causar síntomas más graves, como ictericia, cirrosis hepática e incluso insuficiencia hepática.
La detección temprana de la NAFLD es crucial, ya que permite una intervención oportuna y la prevención de un mayor daño hepático. Para evaluar la condición del hígado, se utilizan pruebas rutinarias de función hepática y estudios de imagen. Las modificaciones en el estilo de vida desempeñan un papel fundamental en el manejo de la NAFLD. La pérdida de peso mediante una combinación de cambios en la alimentación y ejercicio regular ha demostrado ser una opción de tratamiento efectiva.
En los casos en los que la pérdida de peso significativa sea difícil de lograr, la cirugía bariátrica puede considerarse una opción viable. Este procedimiento quirúrgico no solo promueve una reducción sustancial de peso, sino que también mejora los parámetros metabólicos, lo que lleva a una disminución en el contenido de grasa hepática.
El papel de la manga gástrica en el hígado graso
La enfermedad del hígado graso, también conocida como esteatosis hepática, es una afección caracterizada por la acumulación de grasa en el hígado. Puede desarrollarse debido a diversos factores, como la obesidad, el nivel alto de azúcar en la sangre, el colesterol elevado o el consumo excesivo de alcohol. Una de las opciones de tratamiento para la enfermedad del hígado graso es la cirugía de manga gástrica, que consiste en reducir el tamaño del estómago para promover la pérdida de peso. En este artículo, exploraremos el papel de la cirugía de manga gástrica en el manejo de la enfermedad del hígado graso y cómo ayuda a mejorar la salud hepática.
Beneficios de la manga gástrica en el tratamiento del hígado graso
Uno de los principales beneficios de la cirugía de manga gástrica en el tratamiento del hígado graso es su efectividad en la reducción de la grasa hepática. La enfermedad del hígado graso no alcohólico (NAFLD, por sus siglas en inglés) es un trastorno hepático común asociado con la obesidad y puede provocar complicaciones graves si no se trata. Sin embargo, estudios han demostrado que la cirugía de manga gástrica, como la gastrectomía en manga laparoscópica (LSG), puede reducir eficazmente la grasa hepática y mejorar la función del hígado en pacientes con NAFLD.
La LSG es un procedimiento mínimamente invasivo que consiste en la eliminación de una gran parte del estómago, lo que da como resultado una bolsa gástrica más pequeña. Esta reducción en el tamaño del estómago limita la ingesta de alimentos y la absorción de calorías, lo que conduce a la pérdida de peso. Además, se ha encontrado que la LSG tiene un efecto hormonal que potencia la pérdida de peso y reduce el apetito.
El efecto hormonal de la LSG se atribuye principalmente a los cambios en las hormonas intestinales, como la grelina, que regula el hambre y la saciedad. Después de la LSG, los niveles de grelina disminuyen significativamente, lo que reduce el apetito y mejora los resultados de la pérdida de peso. Además, otras hormonas intestinales, como el péptido similar al glucagón tipo 1 (GLP-1) y el péptido YY (PYY), aumentan, promoviendo una sensación de saciedad y potenciando la pérdida de peso.
La manga gástrica ayuda al hígado graso.
¿La manga gástrica puede ayudar al hígado graso? Resumen.
La cirugía de manga gástrica, también conocida como gastrectomía en manga, ha demostrado beneficios potenciales en el tratamiento del hígado graso al reducir la esteatosis hepática y mejorar la enfermedad del hígado graso no alcohólico (NAFLD) en pacientes obesos. Este procedimiento implica la eliminación de una gran porción del estómago para crear un estómago más pequeño con forma de manga, lo que reduce la cantidad de alimentos que se pueden consumir.
La reducción en la ingesta de alimentos y la pérdida de peso resultante de la cirugía de manga gástrica pueden llevar a mejoras significativas en el hígado graso. La acumulación excesiva de grasa en el hígado, conocida como esteatosis hepática, es una característica común de la NAFLD. Los estudios han demostrado que después de someterse a la cirugía de manga gástrica, muchos pacientes obesos experimentan una reducción considerable de la esteatosis hepática y mejoras en la NAFLD.
La investigación sobre los efectos de la cirugía de manga gástrica en la NAFLD ha revelado hallazgos prometedores. Un estudio publicado en el Journal of Hepatology mostró que los pacientes obesos que se sometieron a la gastrectomía en manga demostraron una disminución significativa de la esteatosis hepática después de solo seis meses. Otro estudio publicado en Obesity Surgery mostró resultados similares, con participantes que mostraron mejoras sustanciales en el contenido de grasa hepática tras la cirugía de manga gástrica.